Plantar Plate Tears
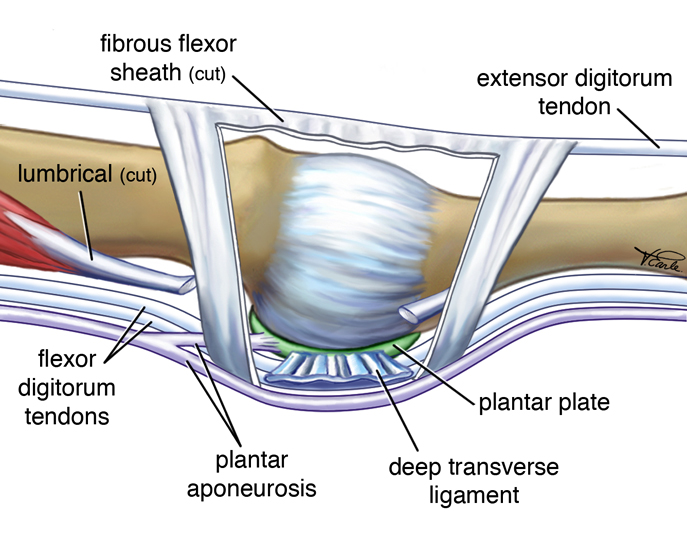
A common forefoot condition seen by podiatrists is an injury to the plantar plate, most commonly under the second metatarsophalangeal joint. The plantar plate is a fibrocartilaginous structure which attaches proximally to the plantar fascia and distally to the base of the proximal phalanx. It also has other ligamentous attachments including the deep transverse metatarsal ligament, the accessory collateral ligament, the proper collateral ligament as well as the extensor hood from the extensor tendons. It’s a highly complex piece of anatomy which is crucial in providing forefoot stability.
Clinically, patients typically present with central plantar forefoot pain, worse on propulsion. Oedema may be seen plantarly and/or dorsally. The floating toe or ‘V’ sign may be seen which tends to accompany partial or complete ruptures of the plantar plate. It can be mistaken for a Morton’s neuroma, but patients with a plantar plate injury typically have pain to palpate at the base of the proximal phalanx, whereas patients with a Morton’s neuroma tend to have pain in the intermetatarsal/interdigital space.
The principles of treatment revolve around reducing the tensile strain of the plantar fascia and plantar plate. This may include digital plantarflexion strapping and a stiff shoe in early stages. We can also make up a forefoot stiffner for the shoe. This may be a 2mm piece of polypropylene in the shape of the forefoot of the shoe, which sits underneath the insole or orthotic.
When prescribing orthoses for patients with plantar plate tears, any orthotic modification which reduces plantar fascia strain will decrease strain to the affected plantar plate. These may include:
Casting/Scanning
- Subtalar joint neutral
- Midtarsal joint fully pronated (this will help to reduce plantar fascial strain)
Cast Modifications
- Pour vertical
- Intrinsic forefoot valgus posting
- Plantar fascia accommodation (3-5mm)
- Consider minimal arch fill
Shell Considerations
- Semi-rigid to rigid materials
- Anterior edge longer to the 2 nd metatarsal
- Intrinsic forefoot valgus shape
- Consider extrinsic forefoot valgus
Top Covers
- Full length
- Soft forefoot extension (e.g. 3.2mm poron)
- Soft top cover (e.g. 2mm multiform)
- An interesting discussion is around the use of metatarsal bars/domes – do these potentially
increase strain through the plantar fascia and plantar plate?
Plantar plate injuries can be a common but at times challenging pathology to manage. By following the above mentioned principles and tailoring your treatment to the individual patient, most patients with this condition can be well managed conservatively.
